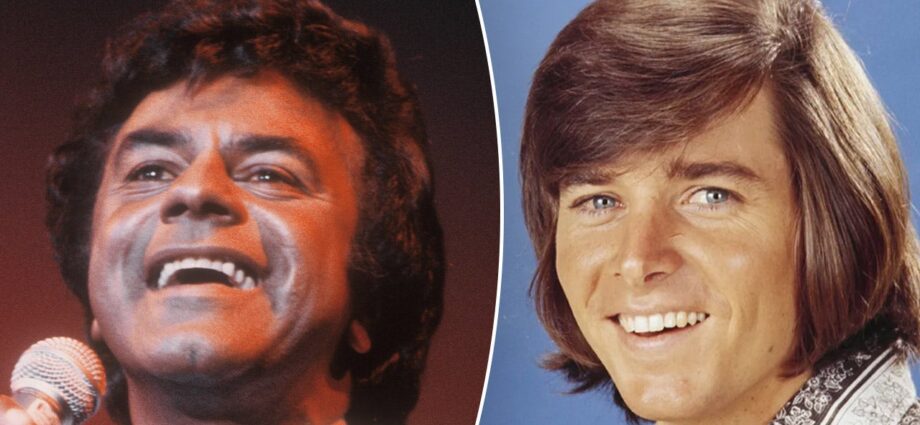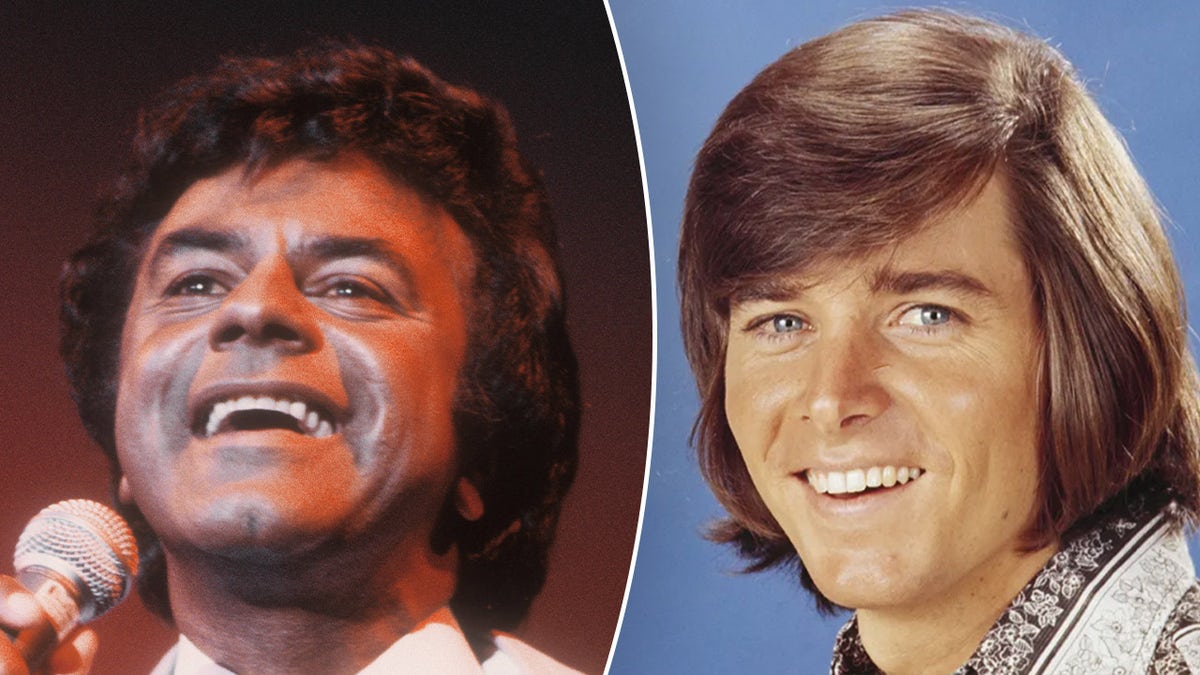
Johnny Mathis shares why he’s retiring from touring; ’60s teen idol Bobby Sherman is battling cancer. (Getty Images)
Welcome to the Fox News Entertainment Newsletter.
TOP 3:
–Johnny Mathis, 89, retires from touring due to ‘accelerated’ memory issues after seven-decade career
-’60s teen idol Bobby Sherman diagnosed with stage 4 cancer
-‘American Pie’ star Tara Reid pushes for a sequel as she hits indie film red carpet

William Shatner scares Gayle King ahead of a space trip with Katy Perry. (Weiss Eubanks/NBCUNIVERSAL via Getty Images)
FINAL FRONTIER – William Shatner shares extreme warnings ahead of Katy Perry, Gayle King’s space flight.
LOVE ON THE LINE – ‘Pawn Stars’ boss Rick Harrison didn’t have prenups for his first 3 wives, unsure if he’d get for his fourth marriage.

King Charles was seen in public the day after his hospital stay due to side effects from cancer treatment. (Yui Mok/PA via AP/Getty Images)
ROYAL RECOVERY – King Charles seen in public the day after a hospital stay for side effects from cancer treatment.
THREE’S COMPANY – Suzanne Somers’ widower used AI to create her ‘twin.’
A-LIST ONLY –Jeff Bezos and Lauren Sanchez’s star-studded wedding guest list is the Who’s Who of Hollywood.

Former “Wheel of Fortune” host Pat Sajak is returning for his “Final Spin.” (ABC/Christopher Willard)
SAJAK’S BACK – Former ‘Wheel of Fortune’ host Pat Sajak to return to the game show for ‘Final Spin.’
‘A MOMENT LIKE THIS’ – ‘American Idol’ winner Kelly Clarkson didn’t know the show was televised when she signed up.
LIKE WHAT YOU’RE READING? CLICK HERE FOR MORE ENTERTAINMENT NEWS
FOLLOW FOX NEWS ON SOCIAL MEDIA